Sleep
Sleep is the third most important health impact for those with pain, so it makes sense to focus your efforts on guiding people to sleep well.
This is not about promising a perfect night’s sleep every night. Your role is to:
- dispel myths by sharing what we know about normal sleep
- share techniques and resources that will help the patient to improve their sleep over a period of weeks

Actions you can take
Get to know all about sleep
Here’s a quick overview of things which can affect the sleep of people living with pain and what might be helpful:
Pain itself
- Mindfulness, progressive muscle relaxation and other distraction techniques have been demonstrated to help people get to sleep and improve sleep quality
Pain medicines
- Review analgesia – does it need a trial of adjusting the dose or formulation to provide some relief overnight. Long-term analgesic use can worsen sleep (opioids especially) so consider if analgesia may be making sleep worse.
- Avoid prescribing sleeping tablets long-term – they can cause rebound insomnia. With these and analgesics, discuss with the person and support them to review their use, how useful the medication is in helping them achieve their goals and plan a slow and steady reduction when they’re ready. As well as improving sleep and pain, reducing unhelpful polypharmacy is known to be beneficial for people’s general health and well-being.
Bedroom comfort
- Bedroom is for sleeping only and best kept dark, quiet and cool
- Do not use any devices that emit blue light, such as smart phones or tablets, in the bedroom. They affect secretion of melatonin from the pineal gland and make it harder to get off to sleep
Mood changes
- Untreated depression or anxiety may contribute to poor sleep. Good treatments are available with both talking therapies and medications.
Lack of routine and daytime inactivity
- Build fitness and activity with a range of different movement activities: walking, stretching, swimming, tai chi, watering plants etc. Moving more often is the key
- Try to set regular times each day for activity and rest
- Set a consistent bed time and rising time (most important)
- Have a consistent bedtime routine
- Stick with this plan for several weeks to allow the body to adapt – even if there are setbacks
Unhelpful thinking about poor sleep
- Lots of worried thinking disrupts sleep. Thinking like about sleep itself, the lack of it, the impact of pain on day to day life and the pain itself. CBT-I is helpful here
- Use relaxation skills e.g. breathing exercises
- Mindfulness resources that aim to improve health and lessen stress are valuable
Side effects of medicines
- Medicines may contribute to day time drowsiness and inactivity and interact with opioids / gabapentinoids so best avoided or only very short term
- Avoid excessive day time napping – this will affect the quality of night sleep
Food and drink choices
- Reduce or cut out caffeine
- If having caffeine, avoid after lunchtime
- Avoid drinking late in the evening if you wake needing to urinate
- Avoid eating large quantities of food late in the evening before sleep time as leads to more restless sleep
- Alcohol and cigarettes can reduce sleep quality
Medical issues
- Obstructive sleep apnoea (OSA) or restless leg syndrome (RLS) may be contributing to poor sleep
Explore the value of mindfulness resources such as apps
These aim to cultivate patience and trust that sleep will come. They do not induce sleep like medicines. Mindfulness works best if practised regularly.
Mindfulness can:
- help break down the vicious cycle of insomnia by guiding attention away from unhelpful thinking and worrying about not sleeping.
- reduce stress and anxiety, which increase our perception of pain; it calms and regulates emotions, decreasing our perception of pain or frustration of not sleeping.
- help greater awareness of thoughts, feelings and body sensations so the person can respond better to the body’s need for rest, balalnce of exercise / activity and healthy eating to maintain a healthy lifestyle.
Resources you can use with the person you are supporting
How to Sleep Well with Pain
This leaflet draws on recent sleep research and provides simple-to-follow guidance for patients to develop the skills they need to start getting a good night’s sleep.
Online resources for people with pain
Meditations for sleep: Headspace website
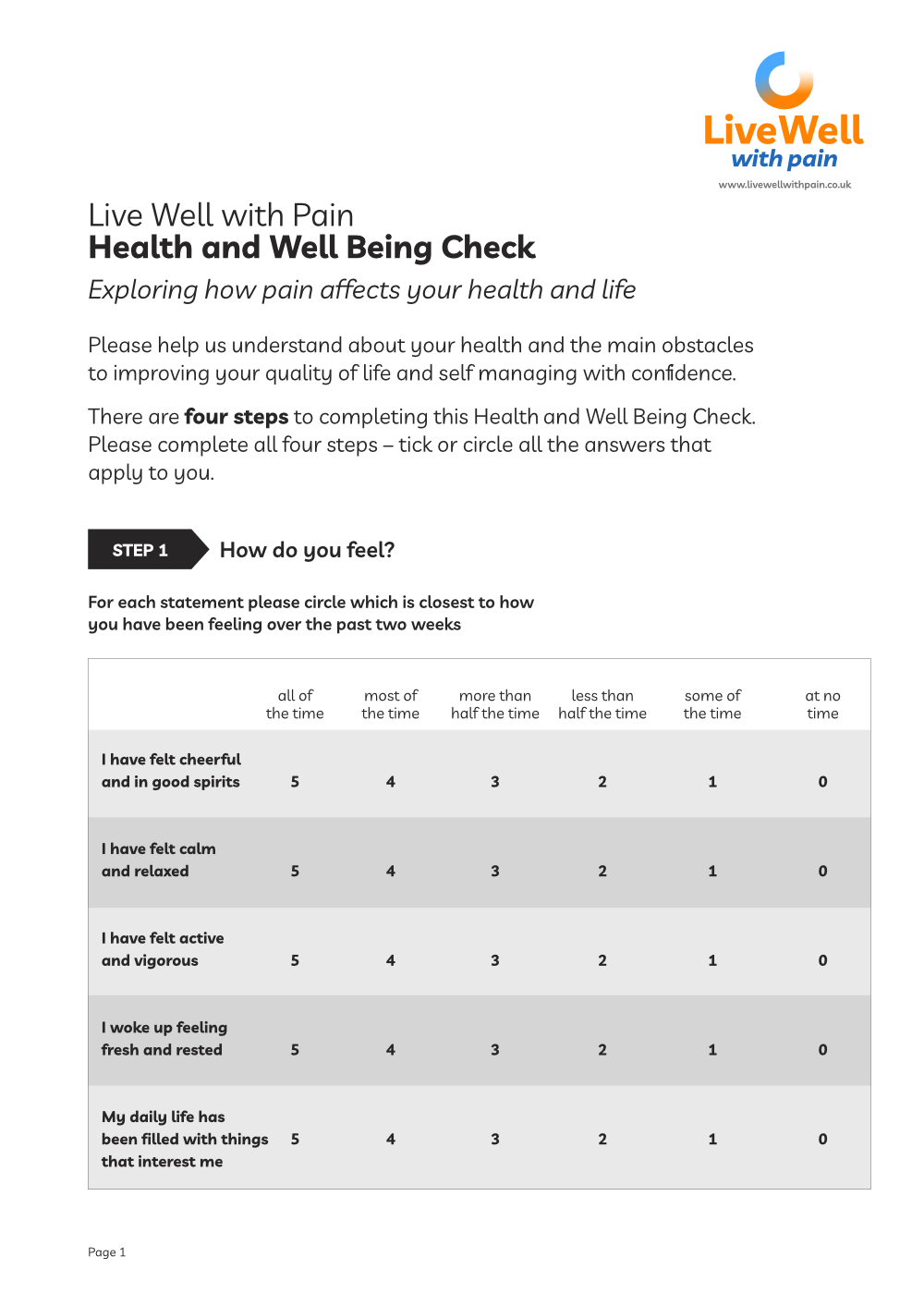
Live Well with Pain Health and Wellbeing Check tool
The Live Well with Pain Health and Well Being Check tool is a self-completion, person-centred tool that can be shared easily with patients and clients.
The data from this completed tool will help identify the actual current impact of chronic pain on the individual and their health.
You can find a more detailed explanation of the Live Well with Pain Health and Well Being Check tool here.
Learning resources for you
Assessing and Managing Sleep Disturbance in Patients with Chronic Pain, in Anesthesiology Clinics Journal
Read the article
Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis
Read the research
Insomnia treatments – the evidence for CBTi
Read on the Sleepstation website
Footstep 6 – Sleep
Summary of key points
✔ Sleep disturbance is common in chronic pain and an important changeable issue. A focus on both pain and sleep management is likely to yield a better outcome
✔ It is important to discuss what normal sleep is for the patient
✔ Sleep hygiene advice, relaxation strategies and CBT have the potential to improve both pain and sleep
✔ It is important to assess and address co-morbid conditions such as depression/OSA/medication side effects
✔ It may also be necessary to explore more on insomnia