Medicines and nutrition
We now know that pain medicines only reduce pain for about 40 percent of people in the long term. And the side effects of pain medicines can have a major impact on your life.
A combination of these side effects, together with being less active because of the pain can lead to becoming overweight. This affects at least 50% of people with pain.
So getting your life back on track often involves making changes with your medicines and your nutrition . . .

1. Medicines
Medicines that people take when they have pain are often referred to as ‘painkillers’. That term might make you think that if you take them, the pain will go. However, pain medicines are unlikely to do that for most people, most of the time.
The reason we use pain medicines is to try to reduce the intensity of the pain you have. Intensity is better described as ‘how much’ pain you feel. If you feel less pain, it should help you to do more of the activities you need to do and those you enjoy.
What are the problems with pain medicines?
There have been large increases in the number of pain medicine prescriptions issued in the UK over the last 20 years.
However, the number of people living with pain is also increasing and the medicines do not seem to be making much difference.
We call pain medicines ‘painkillers’ but now understand that only 4 in 10 people will get much benefit from taking any of them.
For medicines called opioids, which are drugs like codeine, tramadol and morphine, it is likely to be only 1 in 10 people who get benefit.
So, painkillers do not kill pain.
Medicines can actually make things worse
We now realise that opioid medicines especially, can sometimes actually make pain worse.
We think this happens by causing your nervous system to become more sensitive so that pain intensity gets worse – you feel more pain.
All people taking these medicines experience side effects. Sometimes these occur quite soon after starting a medicine or having a dose increased.
However, we now realise many more people are likely to be experiencing long-term side effects from using pain medicines for more than three months.
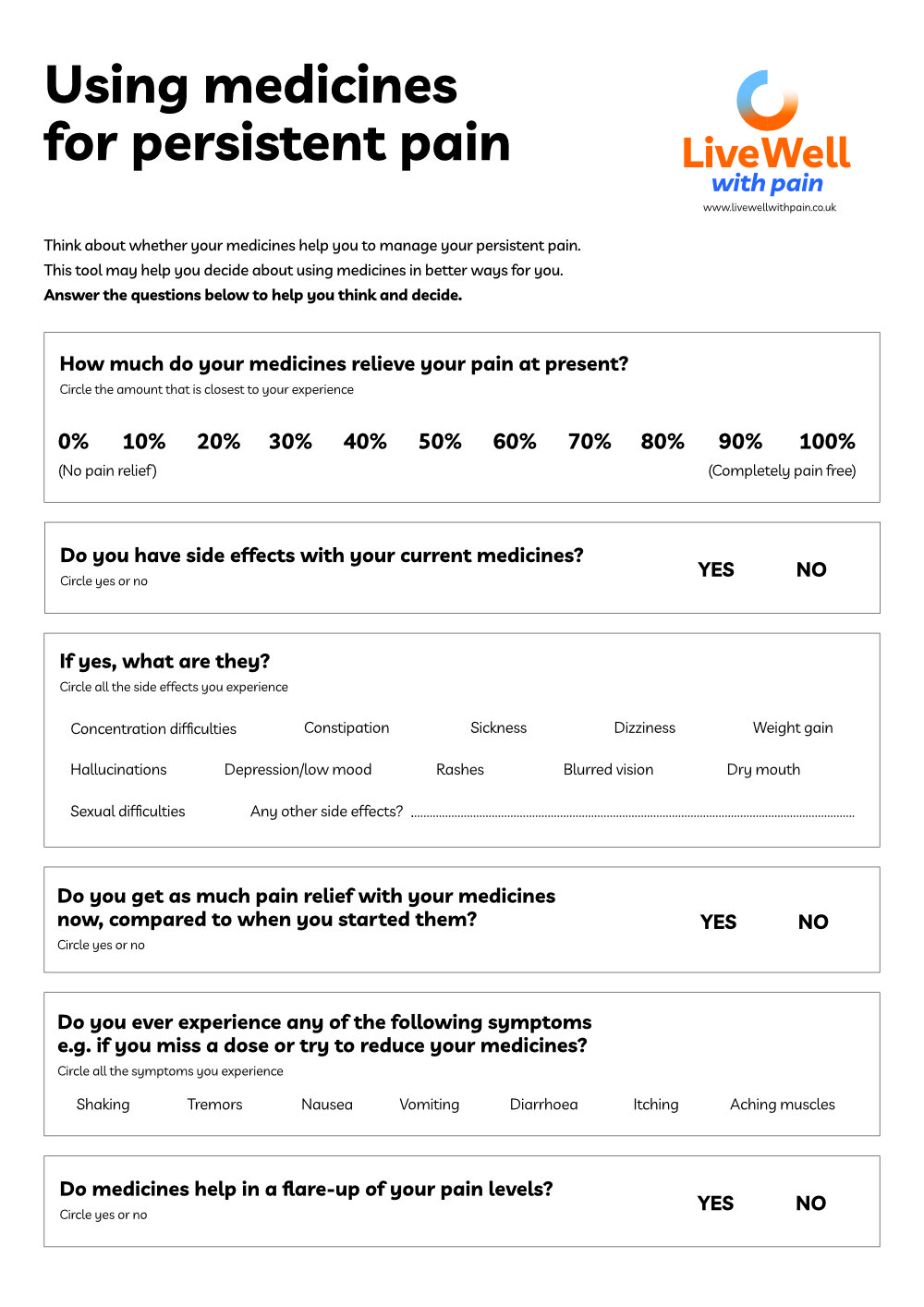
Are you experiencing side effects?
Why are people prescribed pain medicines?
If pain medicines have so many side effects, why do clinicians still prescribe them?
Pain medicines can be helpful for some people. The problem for prescribers, is that it is not possible to tell who might get benefit from taking them and who might not. The important thing is to only continue medicines that are reducing your pain enough to allow you to increase the activities that are important to you and achieve the things you want to do.
This is the main goal of using pain medicines. If they are not reducing the level of pain you experience which then allows you to do more (sometimes called increasing function), then they are likely to be only causing you problems.
How do I know if my medicines are making things harder?
It might sound odd to think that your ‘painkillers’ are not helping to reduce the pain that you feel, especially when you have been taking them for some time.
It may be helpful to think about the problems you are trying to manage – and whether they are caused by your medicines.
What should I do if I am offered a pain medicine?
Make sure you understand what the pain medicine is being prescribed for, the dose, if it will be increased and if so, when.
If you are happy to go ahead
Agree a goal with your prescriber, this might be having a better night’s sleep, getting out for a short walk every day or something else you want to be able to do and that you can manage.
Find out more about doing this in Footstep 4: Setting goals
Agree when the medicine will be reviewed and what you can do if you have any problems in the meantime.
If you are not sure
Never feel that taking a pain medicine is your only option.
Ask your health care team what other options are available – for example: exercise classes, support groups, counselling or psychological support to make sense of your pain experience.
Ask to make an appointment in a week or so, so you can think about it, and discuss it with friends and family before deciding.
Thinking of reducing your pain medicines?
The most important thing to remember is: never stop taking medicines suddenly. Here’s what else you need to know:
I want to reduce my pain medicines >
The good news
The idea of taking pain medicines away may sound worrying – ‘won’t my pain gets worse?’
The majority of people who reduce or stop their medication report that their pain being unchanged or even better than before. They also say that overall, they feel much better as the side effects of the medicines lift, even when they might not have known they had them before making the changes.
If your overall health and wellbeing is better, the intensity of pain is likely to be less. This means you might find it easier to do more. And this also helps reduce how much pain interferes with your day.
‘Most people who reduce or stop their medication report that their pain being unchanged or even better than before’
Life After Opioids
After more than a decade and half of trying – unsuccessfully – to deal with her fibromyalgia through opioids, Louise finally decided that one way or another, she was going to have to manage her pain another way …
In Louise’s words: “I got my life back – I’m living proof that there really is life after opioids!”
(duration: 23 minutes)
2. Nutrition
Being overweight gets people down and affects at least 50% of people with pain. Eating well and having a normal-range weight will help you to build better health and cope well with pain.
Nutrition and pain
New for 2025 is Nutrition and pain – a collection of top nutrition tips and recipes especially designed for people with pain. We’ve even created a handy self assessment tool to help you see how you’re doing with your current diet and explore where you might want to make changes. Check it out here:

Top tips for healthy eating
We asked people living with pain for their key tips on how to improve your diet and reduce weight. Here’s what they came up with:
Do not do yet another weight reduction diet
It can make you feel low even thinking about it!
Medicines for pain can lead to you putting weight on
This is unhelpful and makes managing pain more difficult. So explore options including a medication review with your doctor or pharmacist.
Try and go Mediterranean instead!
Eat more healthy food like pasta, fish, lentils, chicken, vegetables and fruits as these helps joints, muscles and nerves work better. Use olive oil as your main cooking oil as it is healthy oil. Explore more about these foods known as the Mediterranean diet, on the NHS website.
Healthy eating doesn’t just help you lose weight
It also reduces your risk of heart disease, stroke, dementia, cancer, and constipation as well as depression and anxiety.
Low Vitamin D is linked to persistent pain
It’s sensible to take daily supplements as levels can often be low in people with pain. Sunlight helps your body produce Vitamin D, but getting enough is difficult in winter or if you’re indoors a lot. Check with your clinical team and explore NHS Choices to discover more.
Never skip breakfast, as this helps the body be less stressed, tired – and painful!
Start with easy, small portions like two or three tablespoons of cereal or yoghurt or half a banana. People with pain who skip breakfast find eating very small portions is a good start to eating better. Fruit juices and water are healthy too and help reduce drinks with caffeine like coffee and tea.
Eat meals regularly with small portions if you are quite inactive
Snacks can be tempting but unhelpful for managing weight and pain!
Useful resources
Where do medicines fit in?
Informative booklet that explains:
- Why persistent pain happens
- How pain medicines can be helpful as part of your pain management plan
- Some common problems you may experience with these medicines
- When to consider reducing your pain medicines and how to do it
- Other ways of living well with pain

The Great Opioid Side Effect Lottery
Opioids only actually reduce pain for around 10% of people in the long term, and their side effects can be both wide ranging and serious.
This sheet lists many of the side effects, and shows how common they are.
Tick those side effects you are experiencing. You may feel it would be worth asking your GP about reviewing your pain medicines?

Medicines Decision Guide
Are you wondering whether the pain medicines you take are really helping?
Complete this guide and share it with your GP, pharmacist or pain management team. It will help them understand why you may be thinking about continuing, reducing or stopping your pain medicines.
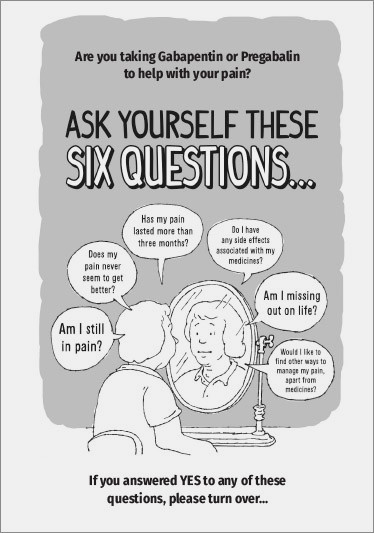
Ask yourself six questions
If you have been taking Gabapentin or Pregabalin to help your long term pain for more than three months, here are six key questions for you.
Patient stories: the harms of opioid prescribing
Two powerful videos that illustrate the harms of strong opioid prescribing in chronic pain.
Faye’s story puts these potential dangers into reality by describing, from her parents’ perspective, the sequence of events that ultimately led to her untimely death from respiratory depression.
Sean’s story describes how strong opioid prescribing had a devastating impact on his quality of life, and how he has engaged with more effective non-drug therapy that has been life-changing.

Medicines and nutrition
Key ideas
✔ Pain medicines only reduce pain for a minority of people in the long term
✔ Side effects are wide ranging and can have a major impact on your life
✔ Reducing your pain medicines – especially opioids – can actually lead to reduction in pain
✔ If you want to reduce your medicines always talk to your prescriber first
✔ Reduce slowly so your body gets used to the change
✔ Healthy eating is also important to how you feel physically and for your mood
✔ A healthy balanced diet can also help you reach a healthy weight
