Managing moods
Mood problems are very common in people with chronic pain. It is important to look out for low moods, negative thinking, anger, anxiety and depression – their ongoing presence indicates greater disability and dependence.
At least 50% of people with chronic pain are depressed so it is worth addressing this changeable factor.
Your role is to ask about these moods regularly and explain how they impact upon the subjective experience of pain.

Actions you can take
1. Identify mood issues
To identify moods quickly, you can use these two questions, adapted for different conditions:
For depression or low mood:
- During the last month, have you often been bothered by feeling down, depressed or hopeless?
- During the last month, have you often been bothered by having little interest or pleasure in doing things?
For anger:
- During the last month, have you often found yourself being angry, irritable or frustrated, every day or some days?
- During the last month, have you found that being angry, irritable or frustrated has interfered with your day-to-day life, affected others or the pain itself?
For anxiety:
Exploring these useful questions can help to understand and guide change in unhelpful avoidant behaviours:
- What have you already been told/think is causing your pain? (beliefs)
- Is there anything that you have been told/think about your pain that you don’t understand or is worrying you? (fears/beliefs)
- How does the pain affect you? (Impact – explore their typical 24 hour period in the last week)
- How does the pain affect your family/those around you? (Wider impact/social support)
- Apart from using medication, how are you managing your pain? (Rest v activity, fear avoidance, beliefs about activity and rest)
- What do you think is going to happen in the future? (Catastrophisation – thinking the worst outcome will happen)
2. Recognise this is different to managing clinical depression
It is important to note that this footstep is not about the management of clinical depression or anxiety. While this is very familiar territory for clinicians with access to clear clinical guidance, it may not be so for others.
The emphasis here is on sharing self-management strategies for day-to-day changes in mood for patients with chronic pain in order to increase their self-confidence to cope.
It is common for people to believe that when mood changes interfere with day-to-day life there is ‘nothing that can be done’ until the mood passes. It is also common for people to blame themselves and believe they ‘should be able to snap out of it’.
Sharing that changes in mood come and go can be helpful. Some people think of this like clouds passing in the sky. Guiding people to be more aware of mood changes and taking some useful actions can make a valued difference. For example doing enjoyable activities such as walking outdoors, listening to music, doing a collage, knitting, going fishing, model making and so on. Isolation is a core issue for people with pain so exploring options for activities with other people is helpful too.
3. Encourage self-care strategies
You can encourage the person you are supporting to use self-care strategies that can help moods to pass quicker and reduce the chances of them becoming entrenched.
If people with pain are struggling with the severity of their moods, depression, anxiety and/or anger then ensure they are linked with clinicians and services for assessment and treatment. Treatment can lead to improvements in these changeable aspects and improve the health and well-being of the person.
Some useful self-care strategies
The five areas model
Encourage people with pain to explore the five areas model from Cognitive Behavioural Therapy (CBT):
The Five Areas Model
Using the five areas model can help a person with pain to see possibilities of change in different areas and focus efforts more effectively.
Practice kindness and self-compassion
This is about encouraging acceptance that none of us are perfect or able to deliver 100% all the time. If we judge ourself against a yard stick of perfection we will constantly come up short and this will promote increased negative thinking and self-judgement. People with pain frequently judge themselves and their lives now with their past and “wish to be what they used to be.”
So, their current life comes up short and they judge from negative unhelpful viewpoint. Being kind and compassionate helps their thinking be more realistic and enable them to take kinder actions for example more balanced pacing of activities and goals.
Notice negative thoughts
and try to balance them with more realistic and positive evidence from the here and now.
Be their own best friend
When these negative thoughts pop into their mind, encourage the person to ask themselves: ‘what would my best friend say at this point to have a balanced perspective?’
Relaxation and mindfulness
Encourage the person to explore and practice relaxation techniques and mindfulness approaches.
Keep a record of positive things that have happened
This will serve as positive real evidence to counter ‘can’t do’ and ‘failure’ thinking. If your patient is unlikely to write things down, this can even be done Instagram-style by taking photos, to make it very easy and low intensity.
Goal setting
Work towards fun goals and things that are meaningful
Peer support
Learn from and get support from peers in a similar situation
Be part of a group
Encourage participation in groups with regular positive focused activities or goals, e.g. a walking for health group, creative or model making, fishing with friends, singing group
Build helpful habits
If something worked one week, then encourage the person to build on it the next week and the next week. Persistence at helpful activities or goals helps build recovery and retrains the brain to manage pain better.
Build in regular enjoyable rewards
Encourage the person to give themselves rewards for making progress in managing moods, progressing goals or other changes.
4. Consider the role of medicines in negatively affecting mood
Medicines like opioids and and gabapentinoids can contribute to low mood.
Medicines may not obviously be a contributing factor to changes in mood especially when mood changes happen over longer periods of time. However, there are some things to be aware of and to discuss with people before starting analgesic medicines when low mood is perhaps already a problem. gabapentin, may cause lowering of mood quite soon after starting it or following a dose change. Opioids however, have been associated with new diagnosis and re-emergence or worsening of pre-exisiting depression but appears to be more common with longer durations of use. Opioids can initially cause a bit of a boost in mood, but this rarely lasts long.
Regular review of analgesic medicines can help pick up problems sooner rather than later. A medicines review to consider all medicines an individual may be using, such as with a pharmacist or GP is a good opportunity to address whether medicines are helping or hindering progress and how they might be affecting a person’s mood more generally.
Resources you can use with the person you are supporting
Self help resources in all formats
A wide range of CBT based resources in all formats: written, audio, MP3 and relaxation exercises:
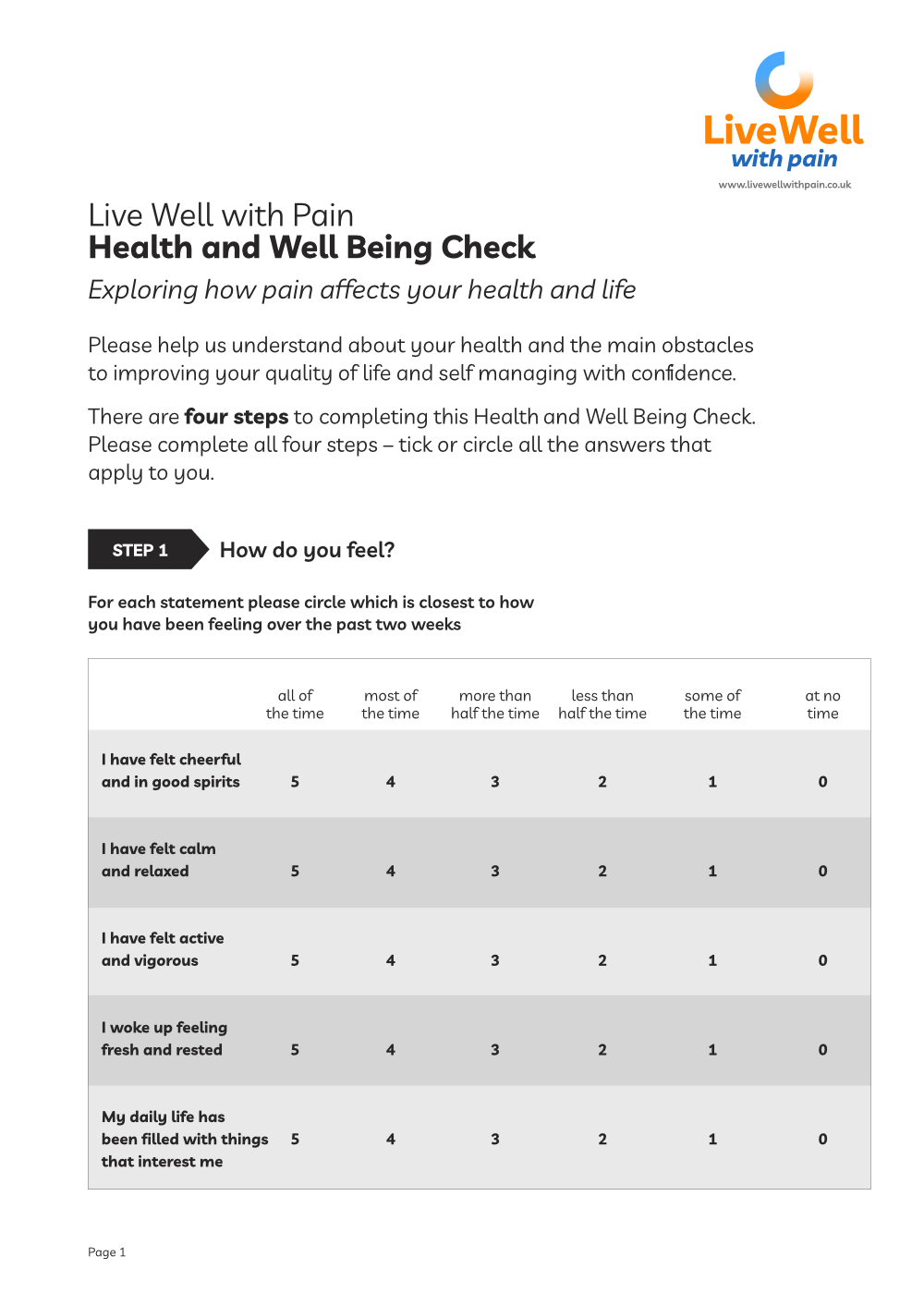
Live Well with Pain Health and Wellbeing Check tool
The Live Well with Pain Health and Well Being Check tool is a self-completion, person-centred tool that can be shared easily with patients and clients.
The data from this completed tool will help identify the actual current impact of chronic pain on the individual and their health.
You can find a more detailed explanation of the Live Well with Pain Health and Well Being Check tool here.
Learning resources for you
Read these interesting papers about where anger, pain and poor outcomes really stand:
Perceived Injustice: A Risk Factor for Problematic Pain Outcomes
Footstep 8 – Managing moods
Summary of key points
✔ Mood impacts on persistent pain and persistent pain impacts on mood
✔ Moods tend to come and go, so it helps people with pain become aware of them and use self-care strategies to lessen their impact
✔ There are plenty of strategies which can help people with pain keep themselves in a positive mood for more of the time
✔ Look for depression and anxiety – if you’re not a clinician with mental health skills, help the person to access services or specialist support
✔ Be aware of the role of medicines such as opioids in contributing to mood changes