Pain and the brain
In this first footstep, as a health care professional working with someone who lives with persistent pain you’ll be looking to engage them with the idea that pain is something that can be tackled in different ways.
Helping people living with pain to understand more about how the brain affects their experience of pain is one way of shifting the conversation away from the medical model and towards a person-focused, self management model.
Your role is to guide the person to realise the need to shift from trying to ‘find and fix’ the pain to ‘managing and living a valued life’ despite the pain.
To do this it may be useful to start by:
- Hearing the pain story from the beginning (particularly if the patient is new to you).
- Reviewing the notes to ensure appropriate indicated medical investigations are complete and any appropriate treatment is optimised.
Note that hearing the person’s story may take a whole appointment – that’s okay. It is important to understand what the person sees at the problems they need support to change. Listening is an intervention in its own right and you should not feel rushed to ‘do’ anything else at that stage. Often it is best to ask the person to come back and pick up the key points in a future discussion rather than try to give information or plan a new treatment.
Listen to the pain story from start to finish
In this short video Dr Tim Williams explains why we need to list to a person’s ‘pain story’ in its entirety.
This is tip number three of Tim’s Ten top tips for clinicians which he recorded a few years ago for Live Well with Pain.
You can watch all ten of Tim’s top tips here.
Once you have listened to the ‘pain story’ you can then help the person to understand that it is time to change the agenda by taking the actions and using the resources described below.
Actions you can take
Share knowledge about pain and the brain
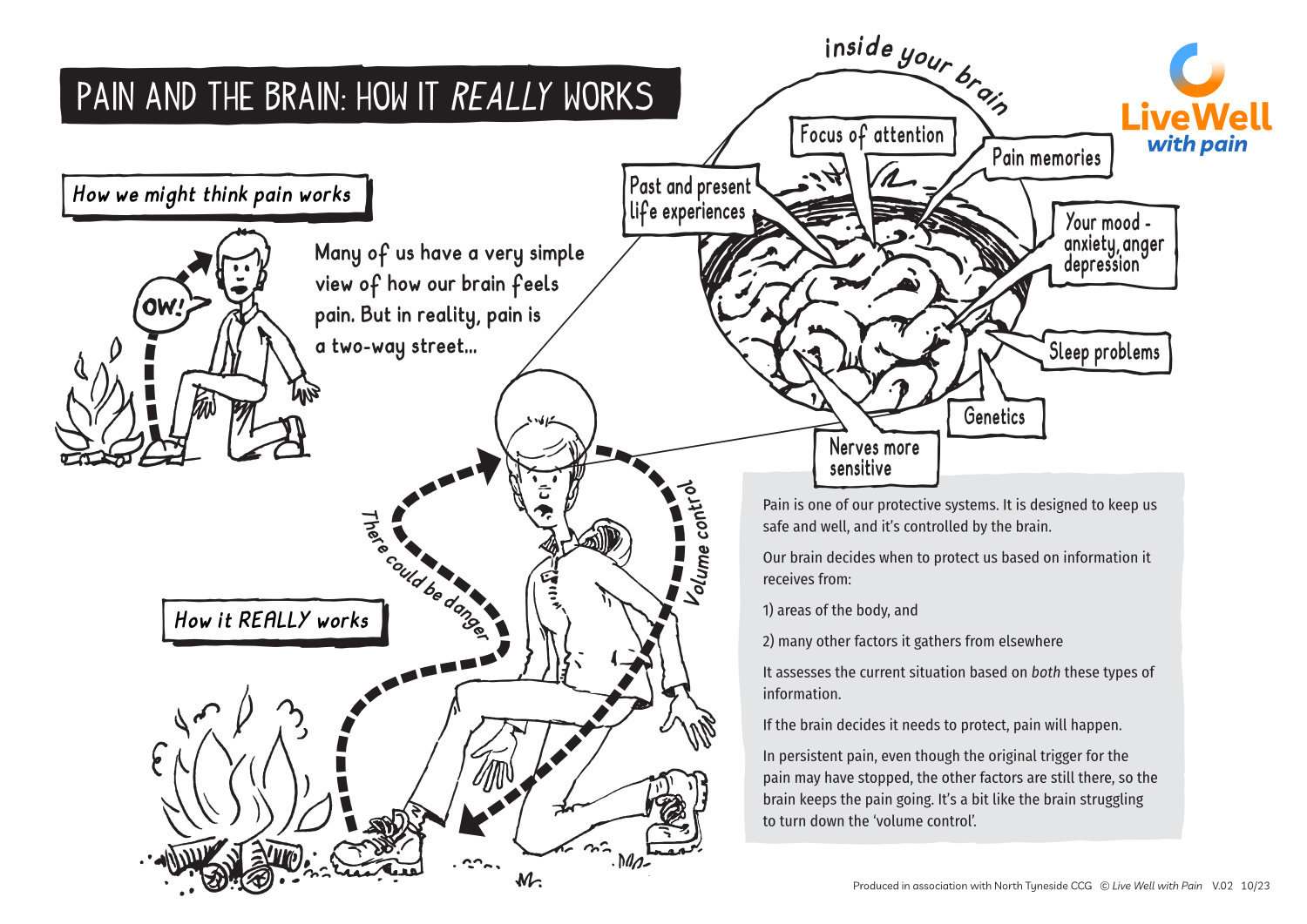
Use the Pain and the Brain sheet to explain the role of the brain in chronic pain. Explain that is it is possible to help the brain to manage pain better, for example by addressing sleep difficulties.
Offer the Explaining Pain leaflet or provide links to videos such as Brain Man.
You can find out more about these resources below.
You could suggest that they look at the information before the next consultation and pick out what they would like to talk through. This may help the discussion about what persistent pain means for them now.
BEGINNER’S TIP
If you are not sure how to explain chronic pain to the person you are working with, you may find the examples of how to broach the subject in these talk bubbles useful.
If you are inexperienced in doing this, consider asking a colleague to role play having this conversation.
Or you could consider video recording yourself in consultation so that you can observe your own and patients’ reactions.

Help the person understand the need to ‘change the agenda’
Shift focus to the changeable
Talk to the person about focusing on things that can be changed, rather than focusing on the pain, which is the least changeable.
Have tools and resources ready
Download and print the pain and self care cycle or Pain is like an iceberg resources to look at with the person (find out more about these resources below).
Exploring these resources together will provide opportunities to open up the conversation and discover areas where they would like to see changes in their lives.
Share stories of success
Use examples from other people with pain who have grown their lives and goals. This evidence that change is posible gives hope. It also helps steer conversations towards the idea of focussing on the changeable.
Resources you can use with the person you are supporting
Pain and the Brain
Many people have a very simple, even simplistic, way of thinking about how and why pain occurs. While this works fine in many day-to-day situations, it falls down when trying to understand persistent pain.
This A4 sheet has been designed to use in consultations with your patient, to help them think about the many factors that are contributing to their experience of persistent pain.
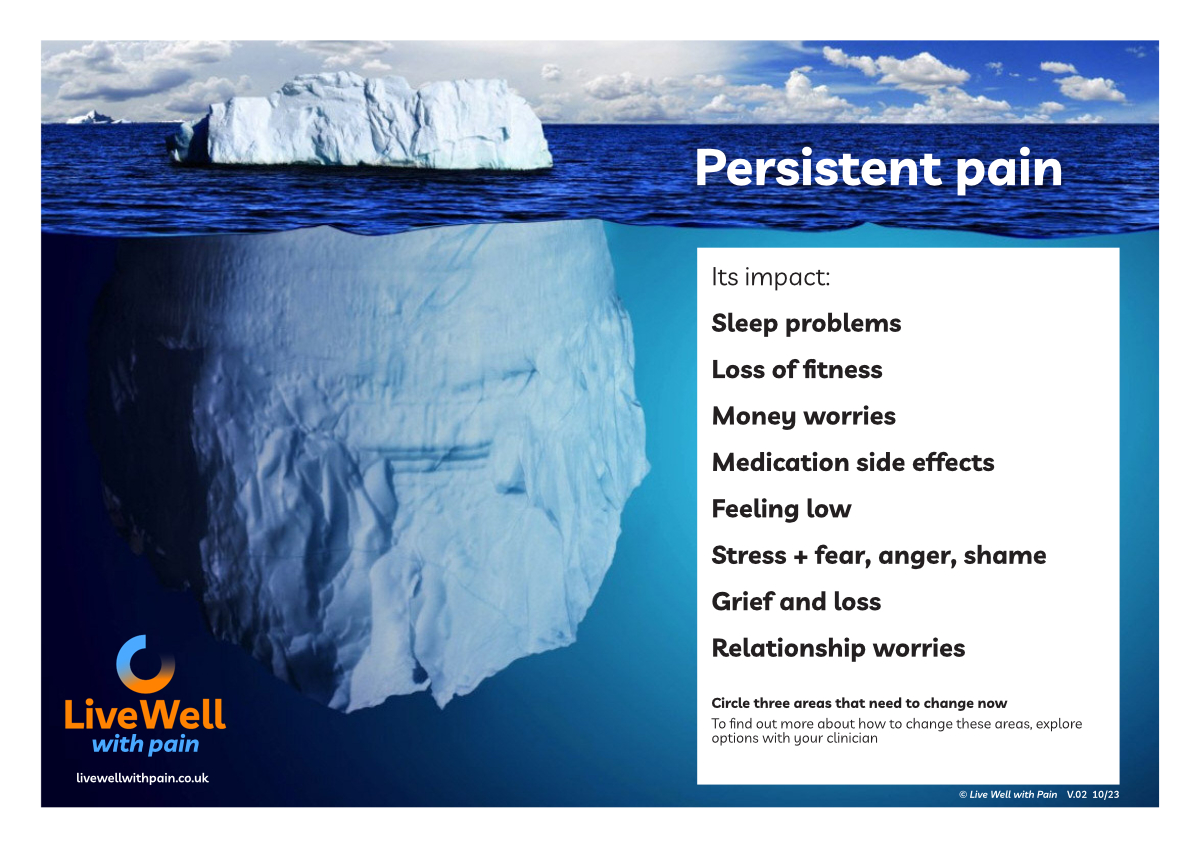
Pain is like an iceberg
Persistent pain is like an iceberg – there’s so much more to it beneath the surface. Use this sheet with your patient to explore how pain impacts many different areas of their life – areas that could be addressed using self management strategies.
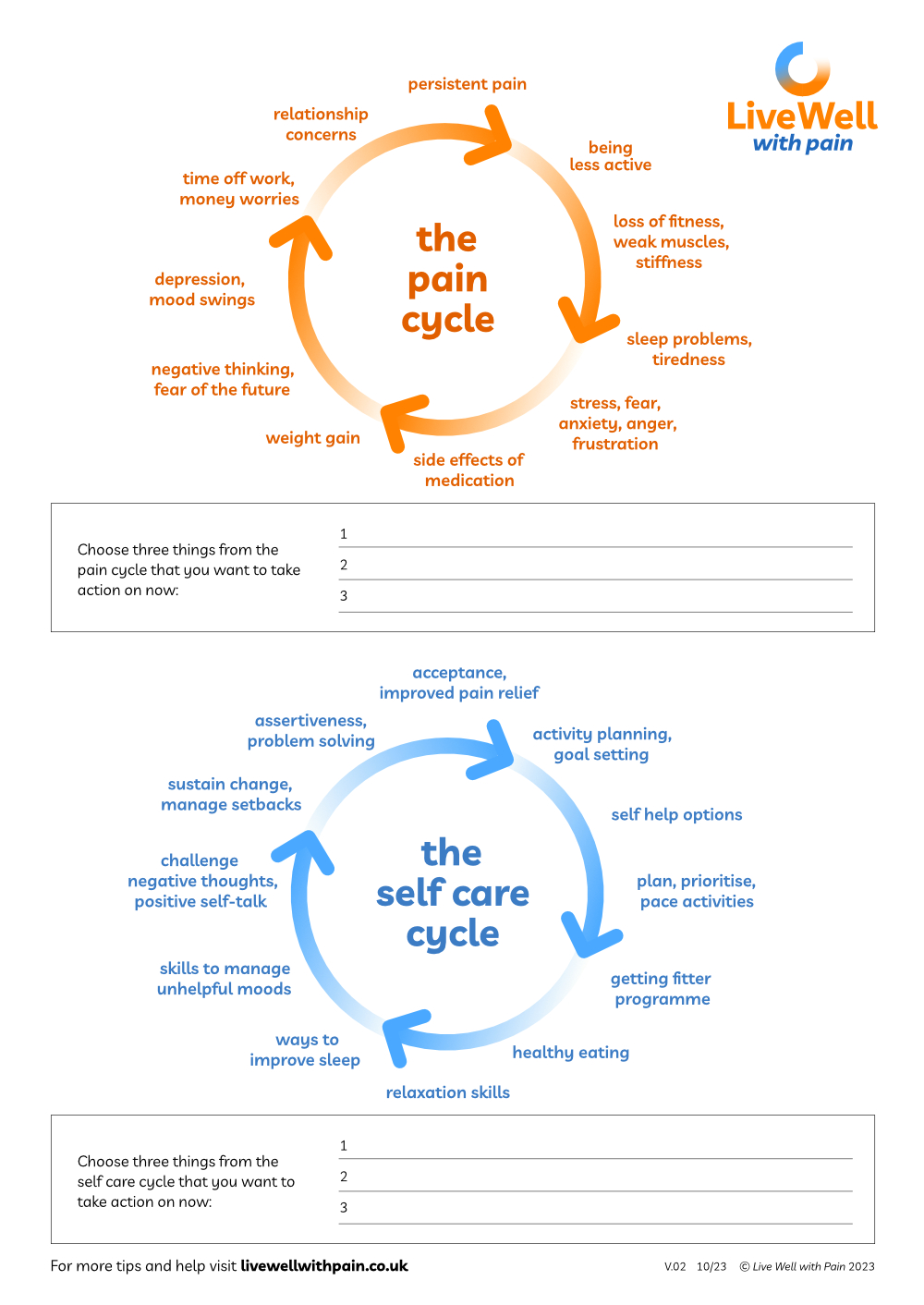
The Pain and Self Care Cycles
Exploring the Pain Cycle with the person you are supporting can help them recognise how pain can affect different aspects of their life in negative and self-reinforcing ways.
Also included is its companion diagram, the Self Care Cycle, which shows the positive outcomes of adopting a range of self-management approaches to undo or limit the impact of pain.
Flippin Pain website
Flippin’ Pain is a public health campaign, with a clear goal: to change the way people think about, talk about and treat persistent pain. Their website has some very useful information to help patients understand more about their persistent pain.

Explaining Pain
This booklet explains: what persistent pain is; what is going on inside us when we experience persistent pain; why people might develop persistent pain in the first place; how it makes us feel; and what we can do about it.
Understand pain in under five minutes
A great little video to share with your patient. Does what it says on the tin.
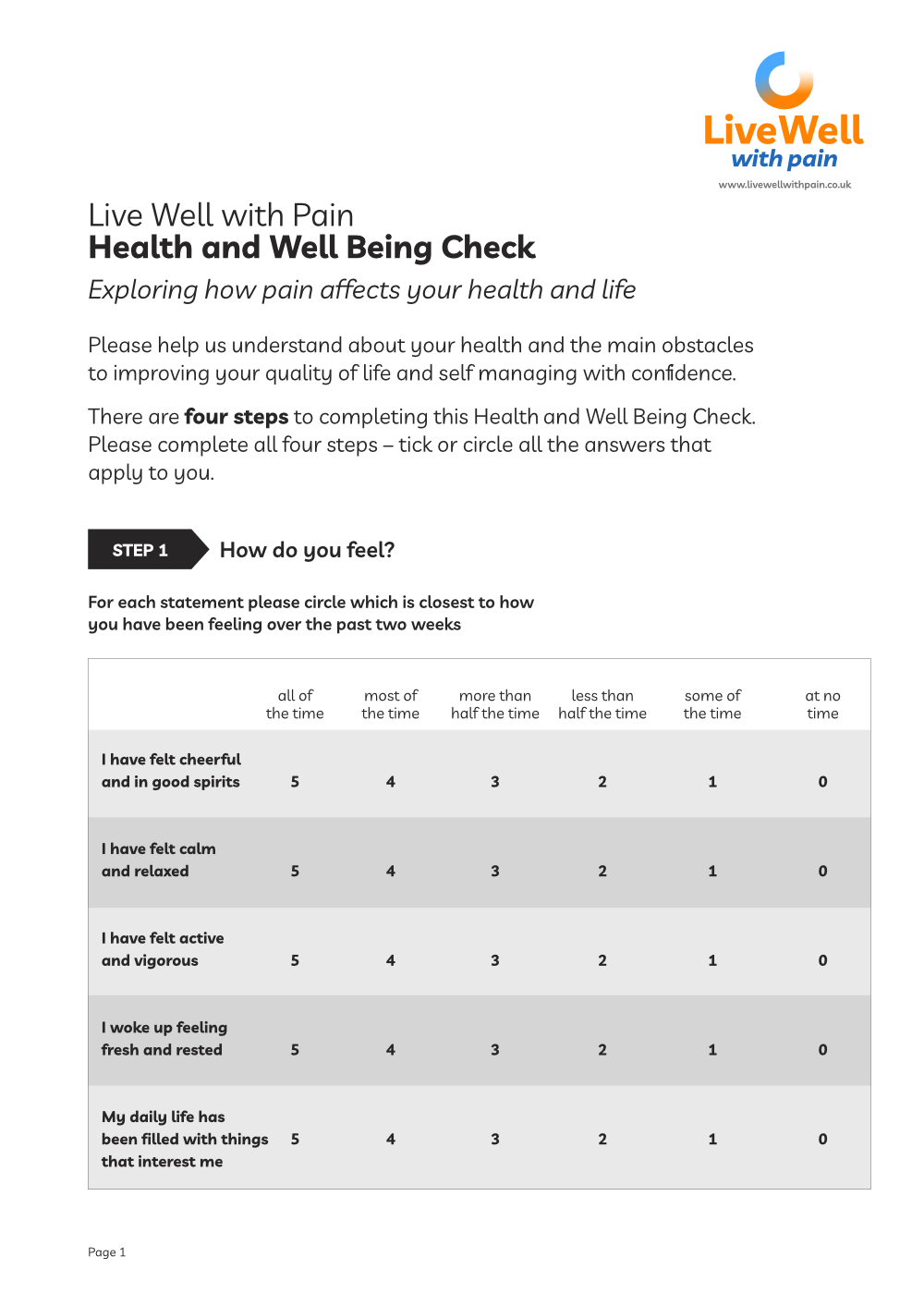
Live Well with Pain Health and Wellbeing Check tool
The Live Well with Pain Health and Well Being Check tool is a self-completion, person-centred tool that can be shared easily with patients and clients.
The data from this completed tool will help identify the actual current impact of chronic pain on the individual and their health.
You can find a more detailed explanation of the Live Well with Pain Health and Well Being Check tool here.
Learning resources for you
Learn more about pain systems here
Understanding pain systems
ICD 11 Classification of chronic pain represents chronic pain as a disease in itself. Chronic secondary pain is chronic pain where the pain is a symptom of an underlying condition:
ICD 11 Classification of Chronic Pain
A useful booklet to help understand persistent pain:
Understanding Persistent Pain
Possibly the best up-to-date talks and information on persistent pain:
Lorimer Moseley on Why Things Hurt
Footstep 1 – Pain and the brain
Summary of key points
✔ An understanding of the relationship between persistent pain and the brain is essential to shifting the conversation away from ‘find and fix’ and towards living well with pain
✔ It will give you and the patient confidence and guide their journey to becoming a self manager of their pain